Mary’s Story – CNAs in Care Planning
What it is: Involving CNAs in care planning means having them as true members of the care team, so that their day-to-day information routinely updates the care plan, and they join in determining the most effective course of action (for implementation guidance and how-to’s, please visit Pioneer Network’s web-based Starter Toolkit and newly released Implementation Handbook for Engaging Staff in Individualizing Care).
Why it is important: CNAs have up-to-date information about residents, know likes, dislikes and customary routines, and can share details of residents’ day-to-day life and activities that families want to hear about at care plan meetings. Residents and families have such strong relationships with and trust in consistently assigned CNAs, that CNAs’ presence makes residents and families more comfortable in the care plan meetings.
How did CNA involvement in care planning help Mary?
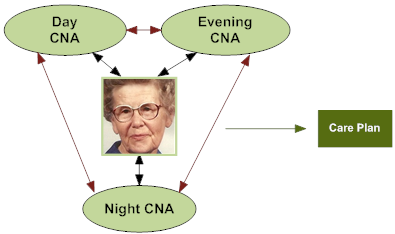
Mary’s CNAs have learned valuable information about her day-to-day preferences and care and have up-to-date information about how she’s doing. They’ve also shared their own individual knowledge with each other to create a “knowledge bank” on what she wants and practices that work. Mary’s caregivers now can work with the clinical team to plug these details into her care plan and get the needed assistance from other departments to accommodate her routines. Information regarding her sleep and eating patterns, ADLs and areas where they are observing risk, such as falls, are discussed and documented PROACTIVELY. They also share concerns regarding what seems to distress Mary, early warnings that she is distressed, and ways to soothe her. Minimizing her distress prevents her from becoming agitated, which in the past would have led to the use of medication to “stop the behavior.”
What might happen WITHOUT CNAs involved in care planning for Mary?
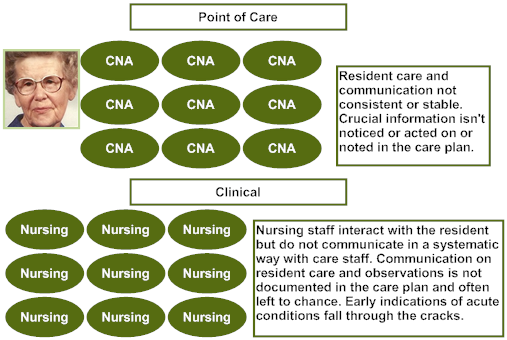
All of the critical information that CNAs readily know about Mary is not integrated with clinical information in her care plan. These details then cannot be used proactively or even in response to an incident (e.g., fall), behavioral expression, or clinical concern. As a result, Mary has been given antipsychotics because causes of, and effective responses to, her distress are not consistently known, shared, and used. Mary is falling now because of the sedative effect of antipsychotic medications. Even with the medications, she is still distressed by staff efforts to redirect her at night and wake her too early in the morning. Clinicians treat her deteriorating condition without realizing that they have caused it by not honoring her customary routines.
Developed by Amy Elliot, PhD, Sonya Barsness, MSG and Barbara Frank. Based on B&F Consulting’s method for Engaging Staff in Individualizing Care, incubated in Pioneer Network’s National Learning Collaborative on Using the MDS as the Engine for High Quality Individualized Care. Funded by The Retirement Research Foundation.

