Communication Map Results
Incubator homes participating with the Pioneer Network Learning Collaborative reported the following outcomes from implementation of consistent assignment, huddles, QI closest to the resident and CNA involvement in care planning:
- Happy Residents – Happy Staff – Incubator homes overwhelming reported this outcome with several using these exact words. Through increased communication, staff now contribute to residents’ quality of life and many garner deep satisfaction from seeing the results for residents.
Teamwork and staff participation – Many homes were energized by the process. One group of homes in New England coined the phrase “huddle mania” to describe the rapid uptake of huddles and positive results. - Communication and relationships – “It’s all about relationships” was another frequently used phrase to describe the changes to organizations through improved resident-staff and staff-staff communication. For many incubator homes, this was a new observation leading to ah-ha moments and a renewed commitment to change.
- Shared problem-solving – Incubator homes found increased communication and shared problem-solving to be a key element in improving quality outcomes. Reductions in antipsychotics, in particular, were reported by homes through sharing information. Staff closest to the residents would work with the clinical team to contribute valuable insights into customary routines and preferences that helped resolve issues and reduce stress for residents with dementia.
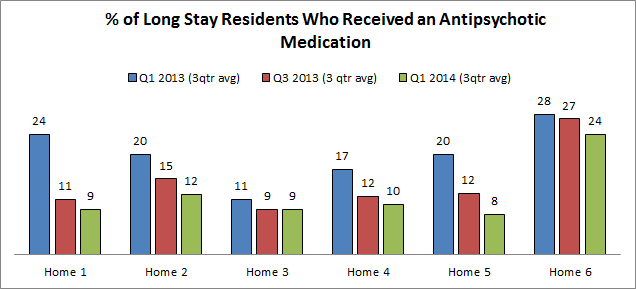
- Clinical outcomes – Through action plans, incubator homes chose specific focus areas for clinical improvement. Homes reported significant reductions in these areas including reductions in restraints/alarms, falls, and the use of antipsychotics. The graph below represents Phase II of the Learning Collaborative where Pioneer Network conducted site visits with a subset of incubator homes to document implementation and sustainability of the four foundational practices. Of the site visit homes, six organizations reported that reductions in antipsychotics were a new initiative through the Learning Collaborative. The descriptive statistics below from Nursing Home Compare represent the pre-Collaborative 3 quarter average from Quarter 1 of 2013, a mid-Collaborative period 6-months later, and a post-Collaborative 3-quarter average. Although some changes were more minor and some were dramatic, each home experienced a reduction through increments of gradual change.
Developed by Amy Elliot, PhD, Sonya Barsness, MSG and Barbara Frank. Based on B&F Consulting’s method for Engaging Staff in Individualizing Care, incubated in Pioneer Network’s National Learning Collaborative on Using the MDS as the Engine for High Quality Individualized Care. Funded by The Retirement Research Foundation.

